

As a health professional, writing progress notes is a time-consuming part of the job. Using tailored models is key to an efficient writing process and standardized notes.
In this article, we'll delve deeper into an effective way for consistently documenting your client's information: SOAP notes.
We’ll explore each component, provide tips and SOAP note examples for effective documentation.
Whether you're new to using SOAP notes or looking to refresh your knowledge, this guide will help you write clear, concise, and comprehensive SOAP notes.
SOAP notes are a widely used method of documentation in the healthcare field, particularly in settings where a client's progress needs to be tracked over time.
The SOAP note format was developed by Dr. Lawrence Weed in the 1960's as a way to organize client information in a structured and concise manner. It was initially used in medical records but has since been adopted across various healthcare disciplines, including mental health, occupational therapy, social work, speech therapy, and more.
One of the key strengths of SOAP notes is their effectiveness in documenting progress and conveying relevant information about the client. Whether you're a mental health counsellor documenting a therapy session, an occupational therapist assessing a client's progress, or a speech therapist tracking a client's language development, the SOAP format provides a systematic approach to documentation.
SOAP stands for:
In addition to the traditional SOAP format, there are variations that offer slightly different structures and focuses that may be taken into consideration when choosing a template.
APSO Notes: The APSO format places the Assessment and Plan first, followed by the Subjective and Objective information. APSO notes are often used in settings where the assessment and plan are the primary focus, and require even easier access.
SOAPE Notes: The SOAPE format adds an Education or Evaluation section after the Assessment. This format is particularly useful when documenting an evaluation of the plan or advice transmitted to the client about various aspects of the treatment process is important.
Ultimately, the choice of format should align with the goals of the documentation and the specific needs of the setting. Whether using the traditional SOAP format or one of its variations, the key is to ensure that the note is organized, concise, and effectively communicates the necessary information for continuity of care or evaluation.
Progress notes are not only a legal requirement for certified mental health professionals, but must also comply with specific standards for both public and private contexts. When writing a progress note, it's essential to consider the following criteria to determine which information to include:
When writing a SOAP note, it’s important to follow the general guidelines for progress notes. The information under each heading should be relevant to the client in question and to the specific consultation context.
Here are some tips for each section:
This section focuses on subjective information that is gathered directly from the client. It should be relevant to the service request and intervention plan. It should not include interpretations and must be verified, with the source clearly identified.
Here, focus on objective observations that can be described clearly as facts. This includes descriptions of behaviours or activities.
In this section, integrate the subjective and objective information gathered in the previous sections to form your professional opinion.
This section allows you to:
In this section, outline the intervention plan and any steps in the client’s treatment, including:
Download our free PDF template to start using the SOAP notes template in your clinical note-taking.
Below are examples of SOAP notes in various clinical contexts. Please note that these are for illustrative purposes only and should not be used for actual clinical documentation.
In mental health counseling, SOAP notes can help document client sessions and track progress, especially with regard to a client's mental health status and treatment plan.
Client reports feeling overwhelmed with work and personal stressors. He describes feeling anxious most of the time and having difficulty sleeping. Client reports increased irritability and difficulty concentrating.
Client's affect is anxious. He appears tense and fidgety during the session. Client's speech is rapid, and he often interrupts himself. Client's body language suggests discomfort.
Client presents with symptoms consistent with generalized anxiety disorder (GAD). Client's symptoms are significantly impacting his daily functioning and well-being. Differential diagnosis includes adjustment disorder with anxiety.
SOAP notes offer a structured approach to documenting client assessments, interventions, and outcomes for occupational therapists. They help facilitate effective communication among healthcare professionals and ensure comprehensive client care.
Client reports increased difficulty in performing activities of daily living (ADLs) due to pain and stiffness in the right shoulder. Client states that the pain has been present for the past month and has worsened over time. Pain is rated as 6/10 on the visual analog scale (VAS).
Client presents with symptoms consistent with adhesive capsulitis (frozen shoulder) of the right shoulder. Pain and stiffness are significantly impacting the client's ability to perform ADLs independently.
Here is an example demonstrating how social workers can use SOAP notes to document client interactions, interventions, and assess needs. In this context, SOAP notes help track progress, facilitate collaboration with other professionals, and ensure effective care.
Client reports feeling overwhelmed with financial stressors. She recently lost her job and is struggling to make ends meet. Client expresses feelings of shame and embarrassment about her current situation.
Client presents with acute stress related to recent job loss and financial instability. Client's feelings of shame and embarrassment are impacting her self-esteem and ability to seek help.
Psylio is a comprehensive recordkeeping platform designed to streamline note-taking, client appointments, and financial management. With built-in templates, such as the SOAP notes template, using Psylio can help you save time and simplify your workflow.
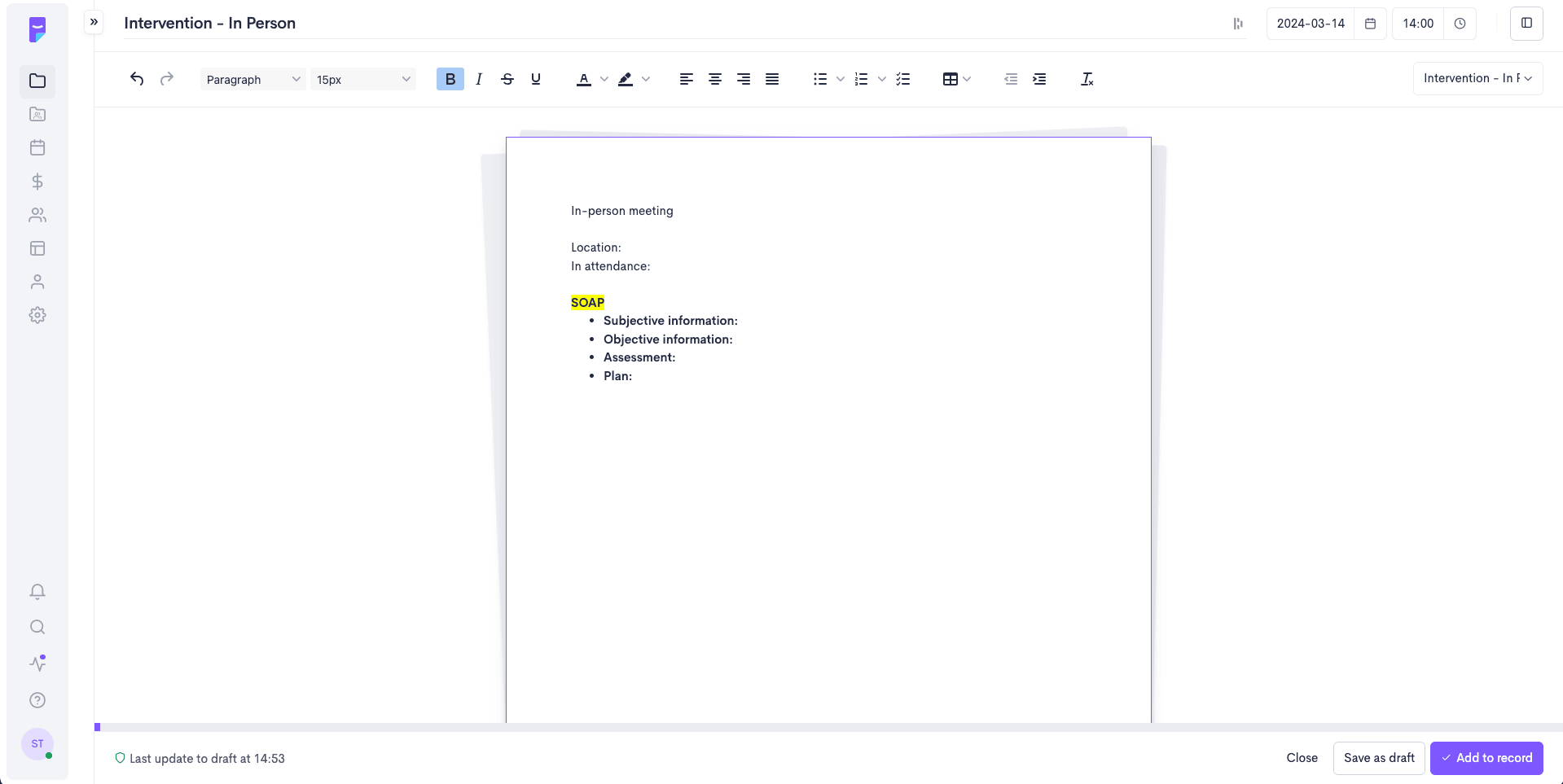
To access the SOAP note template directly integrated into your client progress notes:
A SOAP note is one of several models used in clinical note-taking. And while writing progress notes can be tedious, it's a crucial part of the clinical process.
Using templates based on your preferred models makes progress notes easier to create and ensures standardization across all your notes and among the various professionals in an organization.
Whether you use the templates directly within the Psylio platform or save our free PDF for later use, having access to these tools can free up more time for what matters most - your clients!

Sophie excels as a French and English content specialist and project coordinator for Optania. With a Bachelor of Arts and a double major in French and English literature, her linguistic expertise brings rigour and excellence to the content produced by the team.
Her experience in coordinating content writing, conducting specialized demonstrations and training, and supporting customer service operations demonstrates her continued commitment. Her passion for language and creating quality content is a constant source of motivation in her work.